Understanding the Different Types of Meningitis and How They're Treated
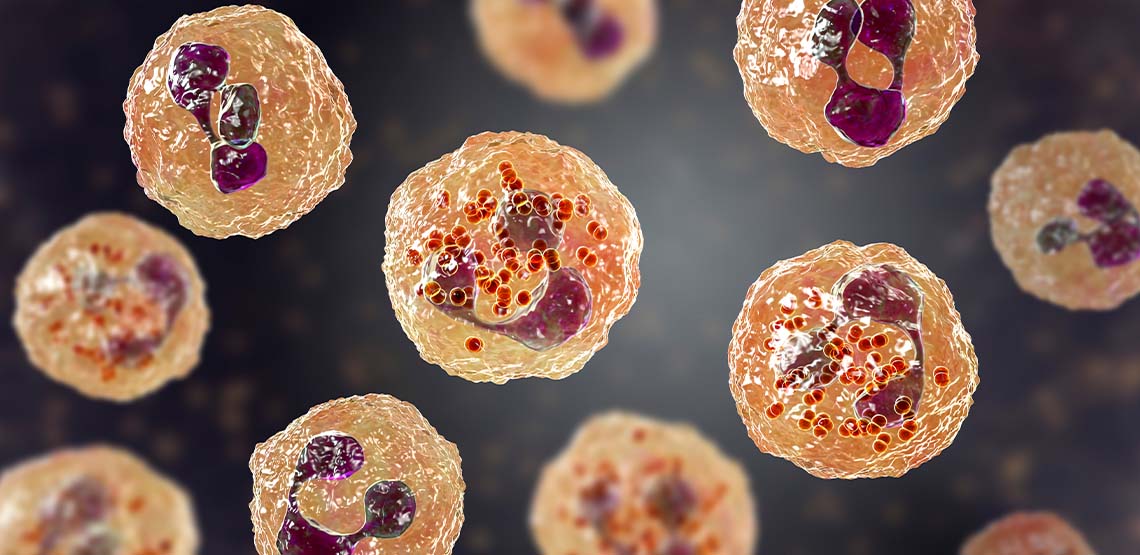
Meningitis is a disease that can be caused by a bacterial, viral, fungal, or parasitic infection. All types of meningitis involve inflammation of the meninges, which are membranes around the spinal cord and brain.
When an infection of these membranes occurs, the resulting symptoms can range in severity depending on the duration, the age of the infected person, as well as the type of meningitis. While meningitis is often treatable, symptoms can be severe and the result can be fatal if left untreated, or even with treatment in some cases. Since severity ranges, acting swiftly if one suspects they or a loved one have meningitis is absolutely crucial.
What Is Meningococcal Disease?
Meningococcal disease is a larger umbrella term that describes any disease, including meningitis, caused by the Neisseria meningitidis bacteria.
Aside from meningitis, meningococcal diseases also include infections in the bloodstream like bacteremia and septicemia, which can be deadly as well. With all types of meningitis, rapid detection and treatment is vital, as is prevention with vaccines.
Causes of Meningitis
The root cause for all types of meningitis is the same mechanism – in the case of viral (most common), bacterial (slightly less common) and fungal infections (least common), a pathogen enters the bloodstream and makes its way to the meninges around the spinal cord and brain where the infection sets in. In the case of viral meningitis, viruses like mumps, herpes, West Nile virus, or HIV, among others, can lead to a case of meningitis.
With bacterial meningitis, there are numerous strains of bacteria that can enter the bloodstream and lead to the infection. Luckily, most are preventable by a vaccine. Examples include the streptococcus pneumoniae bacterium which is a common cause of bacterial meningitis in children (the same bacterium that causes pneumonia or ear infections). Consuming bacteria in the form of cheese or lunch meat can also introduce the bacterium into the blood stream. Bacteria can also be introduced straight into the area around the brain and spinal cord during surgeries, ear or sinus infections, or through a skull fracture.
Less common, noninfectious causes of meningitis are also possible. These include allergies, some types of cancer, chemical reactions and certain inflammatory diseases.
What Are the Risk Factors?
Demographics
Certain risk factors also increase one’s risk for meningitis. Certain demographics, such as college students living in dormitories, are at high risk for contracting meningitis, since living in close contact with others allows for easy transmission (this is why getting vaccinated before college is essential and often required).
Age
Age also matters, as viral meningitis is more likely to occur in those under the age of 5. Bacterial meningitis cases are more common in children and young adults under 20 years of age.
Weakened Immune System
Having a weakened immune system also puts you at greater risk for meningitis. If you have diabetes, AIDS, or take immunosuppressant drugs, you are statistically at higher risk for contracting the disease.
While the most common types of meningitis— fungal and bacterial—are very contagious and can easily transmit in schools, dormitories, army bases or just person to person, fungal, parasitic and noninfectious meningitis are not contagious.
What Are the Symptoms?
Classic symptoms of meningitis to know and keep an eye out for in yourself and others:
- Headache
- Stiff neck
- Fever
These can emerge after a primary illness such as the flu, but they can also emerge seemingly out of nowhere and with very little warning. They can develop in a matter of hours and demand rapid treatment.
Less common but other possible symptoms include drowsiness, acting confused or even silly, nausea, lack of appetite, or sensitivity to light. Being aware of these symptoms may help save your life or a loved one’s.
Related Search Topics (Ads)
Consequences and Complications
If left untreated, or even in some cases with treatment, meningitis can ultimately result in death. This is why getting properly vaccinated is so essential in preventing meningitis, since many types have a high death rate even with all proper medical intervention.
Aside from death, there are other complications of meningitis:
- Seizures
- Headaches
- Brain damage
- Memory loss
- Hearing loss
- Vision loss
The Diagnostic Process
In order to diagnose meningitis, visit your healthcare provider as quickly as possible. During the visit, physical symptoms will be assessed and telltale signs of meningitis, such as a fever and stiff neck, will be checked for. A spinal tab or lumbar puncture is also a vital step in diagnosis since this allows a doctor to test for inflammation or bacteria around the spinal cord and brain. Other methods of diagnosis include blood tests that can detect the presence of meningitis-causing bacteria.
How to Prevent Meningitis
To prevent meningitis, a twofold approach of vaccines plus basic hygiene habits are extremely important. Basic steps like washing hands, not sharing utensils or drinking or eating after others, and covering your mouth when sneezing and coughing can help prevent the spread. Keeping yourself healthy by getting plenty of sleep, eating healthy food and avoiding smoking are also vital.
There are several types of vaccines to prevent many of the types of meningitis, so speak with your healthcare provider to make sure you are up to date on yours. Children routinely receive many and older adults are advised to get others, as are teenagers before heading off to college.
Meningitis Treatment
If your doctor determines you have a form of meningitis, they will treat it based on the type.
Viral Cases
For viral cases, many will resolve on their own and antibiotics will not have any affect. Your doctor will prescribe plenty of rest, fluids and may help keep you comfortable with pain medication and corticosteroids to bring brain swelling down.
Bacterial Cases
In bacterial cases, more aggressive treatment is necessary including hospitalization where the patient will be treated with antibiotics and oftentimes also given corticosteroids to prevent brain swelling. This can prevent further complications or even death.
Fungal Cases
In fungal meningitis an antifungal is used and parasitic meningitis treatment depends on the cause, but treatment may involve antibiotics.